July 4, 2025, marks a critical juncture for Artificial Intelligence in healthcare, as groundbreaking advancements in AI-powered diagnostics are met with a growing call for stronger ethical frameworks, particularly concerning patient consent.
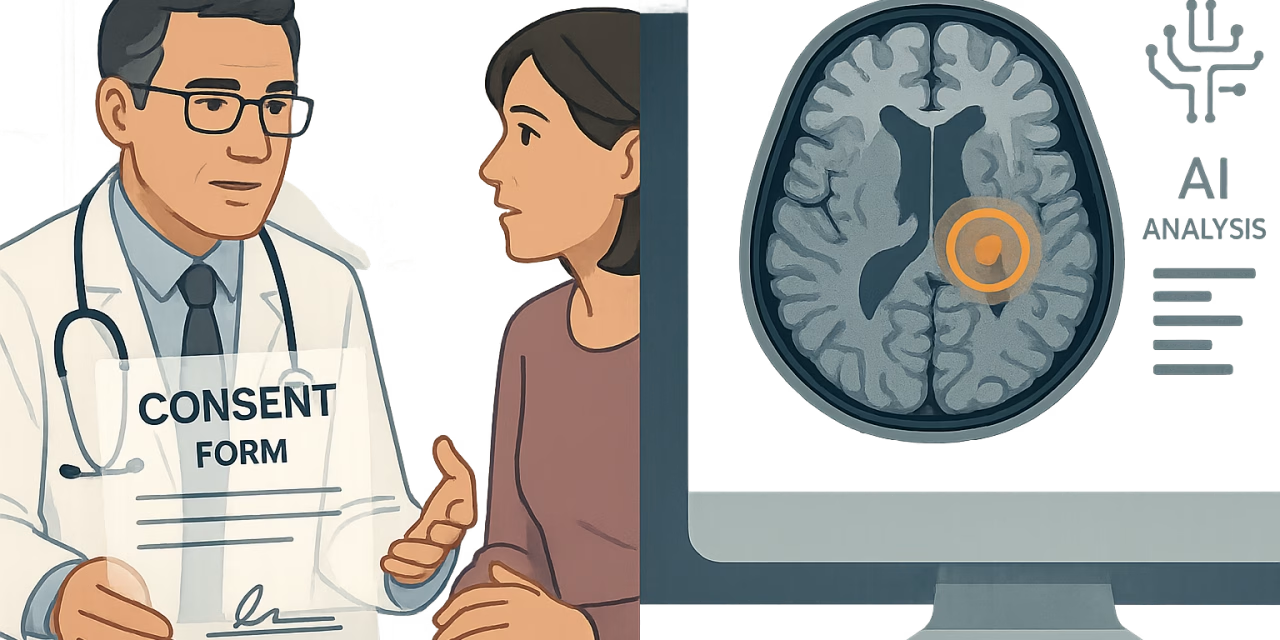
A study published in BMC Medical Ethics urges medical institutions to adopt explicit patient consent protocols when using AI in clinical decisions. The authors warn that vague disclosures undermine patient autonomy and trust, and they call for transparent frameworks and accountability mechanisms for AI-assisted care. This highlights the urgent need to ensure that as AI becomes more integrated into healthcare, the fundamental rights and autonomy of patients are protected.
This ethical debate is unfolding alongside remarkable technological breakthroughs. On July 5, a study in Nature Communications demonstrated that AI models can accurately estimate brain age from MRI scans, a method that could aid in the early diagnosis of neurodegenerative conditions. Another study showed an AI model achieving over 90% accuracy in detecting diseases like cancer in their early stages by analyzing patient history, imaging data, and biomarkers.
These advancements showcase AI’s immense potential to revolutionize preventive care and improve patient outcomes. However, they also underscore the importance of the ethical considerations raised by bioethicists. As AI systems become more capable of making complex medical assessments, the need for clear communication and informed consent becomes paramount.
The launch of the WHO Collaborating Centre on AI for Health Governance in Rwanda further emphasizes the global commitment to establishing standards for the safe and ethical use of AI in healthcare. The developments on July 4, 2025, collectively illustrate that the future of AI in health and wellness will be shaped not just by technological innovation, but by a parallel commitment to ethical principles that prioritize patient trust and autonomy.